
During a hernia operation, Dorothea Handron's surgeon unknowingly pierced her bowel. It took five days for doctors to determine she had an infection.
By the time they operated on her again, she was so weakened that she was placed in a medically induced coma at Vidant Medical Center in Greenville, N.C. On a respirator for six weeks, she contracted pneumonia.
"When they stopped the sedation and I woke up, I had no idea what had happened to me," said Handron, 60. "I kind of felt like Rip Van Winkle."
Because of complications like Handron's, Vidant, an academic medical center in eastern North Carolina, is likely to have its Medicare payments docked this fall through the federal government's toughest effort yet to crack down on infections and other patient injuries, federal records show.
A quarter of the nation's hospitals -- those with the worst rates -- will lose 1 percent of every Medicare payment for a year starting in October. In April, federal officials released a preliminary analysis of which hospitals would be assessed, identifying 761.
When Medicare sets final penalties later this year, that list may change because the government will be looking at performance over a longer period than it used to calculate the draft penalties. Vidant, for instance, says it lowered patient injury rates over the course of 2013, and Handron praises its efforts.
The sanctions, estimated to total $330 million over a year, kick in at a time when most infections measured in hospitals are on the decline, but still too common. In 2012, one out of every eight patients nationally suffered a potentially avoidable complication during a hospital stay, the government estimates.
Related: Hospitals profit more from surgical complications - report
Even infections that are waning are not decreasing fast enough to meet targets set by the government. Meanwhile new strains of antibiotic-resistant bacteria are making infections much harder to cure.
Dr. Clifford McDonald, a senior adviser at the federal Centers for Disease Control and Prevention, said the worst performers "still have a lot of room to move in a positive direction."
Are The Metrics Right?
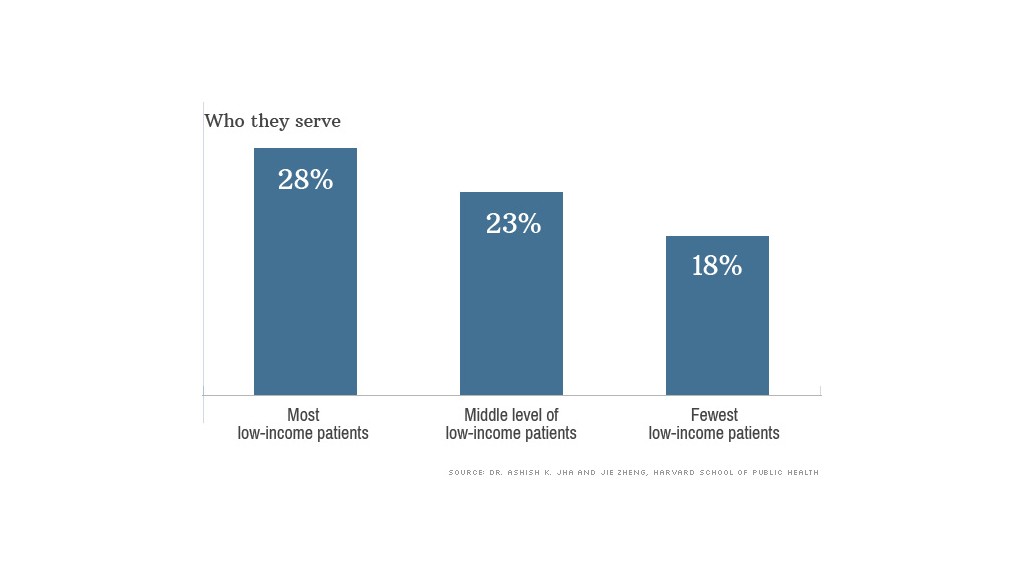
Medicare's penalties are going to hit some types of hospitals harder than others, according to an analysis of the preliminary penalties conducted for Kaiser Health News by Dr. Ashish Jha, a professor at the Harvard School of Public Health. Publicly owned hospitals and those that treat large portions of low-income patients are more likely to be assessed penalties. Preliminary penalties were assigned to more than a third of hospitals in Alaska, Colorado, Connecticut, the District of Columbia, Nevada, Oregon, Utah, Wisconsin and Wyoming, Medicare records show.
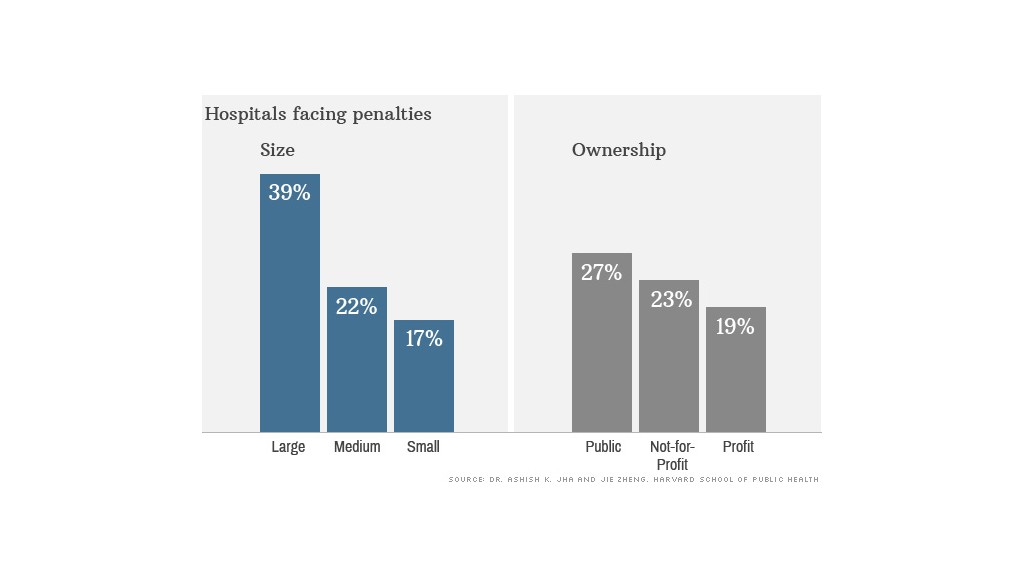
The biggest impact may be on the nation's major teaching hospitals: 54% were marked for preliminary penalties, Jha found. The reasons for such high rates of complications in these elite hospitals are being intensely debated.
The government takes into account the size of hospital, the location where the patient was treated and whether it is affiliated with a medical school when calculating infection rates. But the Association of American Medical Colleges and some experts question whether those measures are precise enough.
"Do we really believe that large academic medical centers are providing such drastically worse care, or is it that we just haven't gotten our metrics right?" Jha said. "I suspect it's the latter."
Medicare assigned a preliminary penalty to Northwestern Memorial Hospital in Chicago, for instance, but Dr. Gary Noskin, the chief medical officer, said hospitals that are more vigilant in catching problems end up looking worse.
"Hospitals that have been working hard to reduce infections may end up in the penalty box," said Nancy Foster, vice president for quality and public safety at the American Hospital Association.
Third Leg Of Medicare's Pay-For-Performance
The Hospital-Acquired Condition (HAC) Reduction Program, created by the 2010 health law, is the third of the federal health law's major mandatory pay-for-performance programs for hospitals. The first levies penalties against hospitals with high readmission rates and the second awards bonuses or penalties based on two dozen quality measures. Both are in their second year.
When all three programs are in place this fall, hospitals will be at risk of losing up to 5.4% of their Medicare payments.
Related: Medicare payment rates: $15,000 for one hospital, $26,000 for another
In the first year of the HAC penalties, Medicare will look at three measures. One is the frequency of bloodstream infections in patients with catheters inserted into a major vein to deliver antibiotics, nutrients, chemotherapy or other treatments. The second is the rates of infections from catheters inserted into the bladder to drain urine. Both those assessments will be based on infections during 2012 and 2013.
Finally, Medicare will examine a variety of avoidable safety problems in patients that occurred from July 2011 through June 2013, including bedsores, hip fractures, blood clots and accidental lung punctures.
"With infections, we are moving in the right direction," said Lisa McGiffert, who directs the patient safety program at Consumers Union, "but I would not say we are anywhere near where we need to be."
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation.


