Prescription drug manufacturers dole out billions of dollars in rebates every year, but these savings don't usually trickle down directly to consumers.
That may change if the Trump administration has its way. Officials are looking to require insurers to pass at least part of these concessions along to Medicare beneficiaries, which could prompt changes in the broader insurance market as well.
Drug rebates have become an essential, but opaque part of the pharmaceutical industry. However, they are now in the spotlight as the Trump administration seeks ways to lower drug prices. President Donald Trump is expected to give a speech this week on drug prices, with rebates playing a central role.
"There's a range of reasons why drug prices are too high," Scott Gottlieb, commissioner of the Food & Drug Administration, said at the Food and Drug Law Institute conference last week. "To take one example, one of the dynamics I've talked about before that's driving higher and higher list prices, is the system of rebates between payers and manufacturers."
Like most things in America's health care system, it's exceedingly difficult to know just how much a medication costs or what different players in the supply chain pay or earn along the way.
Related: How Trump plans to cut prescription drug prices
Here's what we know about drug rebates:
Insurers hire pharmacy benefit managers to administer drug programs for their clients, including employers and federal and state governments, who provide drug coverage through Medicare and Medicaid managed care plans.
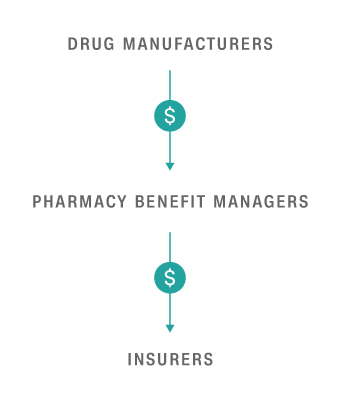
The managers negotiate rebates from drug manufacturers to insurers in exchange for better coverage terms -- often in the form of lower co-pays for brand name drugs. This makes it more likely that policyholders will choose that cheaper brand name medication over a competitor's version. These middlemen, however, also keep a portion of the rebate for themselves.
The rebate figures are eye-popping. Insurers received $89 billion in rebates, reducing their spending on prescription drugs to $279 billion in 2016, according to estimates from Altarum, a research and consulting firm. This doesn't include the portion of the rebate that pharmacy benefit managers keep, which isn't disclosed.
Insurers argue that they pass along the savings to consumers in the form of lower premiums and out-of-pocket costs. And the Pharmaceutical Care Management Association, which represents the managers, says that the rebates help keep drug spending in check even as list prices increase.
"These rebates are used by payers to reduce premiums and out-of-pocket costs for patients," the association said in response to Gottlieb's remarks. "Getting rid of rebates would leave patients and payers, including Medicaid and Medicare, at the mercy of drug manufacturer pricing strategies."
Related: UnitedHealthcare will pass along drug discounts to some customers
But the system has come under scrutiny, both for the lack of transparency and for the burden it places on consumers. Policyholders' co-pays are typically based on the list price of the drug, not the cost after the rebate.
Some insurers are already changing their ways. UnitedHealthcare (UNH) and Aetna (AET) said in March that they would pass along the rebates to their customers enrolled in a certain type of job-based insurance coverage. It would affect a total of about 10 million policyholders at the two carriers.
UnitedHealthcare said the discounts can range from a few dollars to more than $1,000 per prescription, depending on the medication. The company also said the move would not lead to increased rates. Aetna did not provide such details.
Related: Some Aetna customers will see lower drug prices
Passing along the rebate, however, will benefit relatively few Americans, said Gerard Anderson, a health policy professor at Johns Hopkins University. It will likely lower -- or even eliminate -- the co-pays for those taking expensive brand name drugs for serious conditions, such as cancer, diabetes or hepatitis C. (Insurers generally don't receive rebates for generic drugs, which made up 89% of prescriptions but only 26% of drug spending in 2016, according to the Association for Accessible Medicines, the trade association for generic medicines.)
Shifting the rebates, however, could raise costs for everyone else, both because insurers could raise premiums to make up for the loss of the discounts and because sicker patients will likely take even more of the pricey medications if they don't cost much.
"Lower co-pays on the part of consumers mean insurers are paying more," said Ani Turner, co-director of sustainable health spending strategies at Altarum. "If that results in higher premiums, it's not clear if consumers overall will benefit."


